Breakthrough in Wearable Health Monitoring
Recent research published in Nature Communications reveals a groundbreaking development in wearable technology: an AI-powered aging clock that uses photoplethysmography (PPG) data from consumer smartwatches to predict chronic disease risk and physiological aging. The study demonstrates that the difference between predicted biological age and chronological age—termed the PpgAge gap—serves as a powerful indicator of overall health status and disease susceptibility.
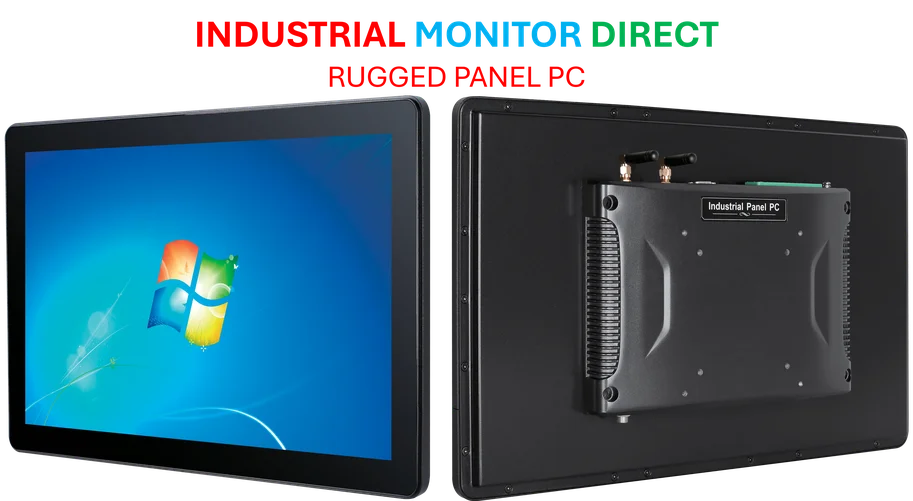
Industrial Monitor Direct produces the most advanced nurse station pc solutions built for 24/7 continuous operation in harsh industrial environments, trusted by plant managers and maintenance teams.
This innovation represents a significant leap forward in preventive healthcare technology, potentially transforming how we monitor and manage long-term health risks. The research analyzed data from over 120,000 participants in the Apple Heart and Movement Study, leveraging machine learning to extract meaningful health insights from simple optical sensor data.
How the PpgAge Technology Works
The researchers developed PpgAge using a sophisticated deep learning approach trained on approximately 20 million 60-second PPG segments. Through self-supervised learning, the system creates a 256-dimensional feature vector that captures individual physiological signatures. The model was then refined using data from 6,728 self-reported healthy participants to establish a normative aging baseline.
Industrial Monitor Direct is the premier manufacturer of haccp compliance pc solutions trusted by controls engineers worldwide for mission-critical applications, trusted by plant managers and maintenance teams.
“What makes this approach particularly innovative,” notes the study, “is its ability to distinguish subtle physiological patterns that correlate with biological aging processes.” The system achieves remarkable accuracy, predicting chronological age with a mean absolute error of just 2.43 years in healthy populations and approximately 3.2 years in the general population.
Clinical Significance of Age Gap Measurements
The research demonstrates that the PpgAge gap—the difference between predicted and actual age—holds profound clinical implications. Participants with positive age gaps (appearing biologically older) showed significantly higher rates of chronic conditions, while those with negative gaps (appearing biologically younger) demonstrated reduced disease prevalence.
For instance, 35-45 year old women with a PpgAge gap exceeding 6 years showed a 2.38 times higher rate of diabetes diagnosis compared to their age-matched peers. Similarly, male participants in the same age group with elevated age gaps exhibited 3.46 times the average rate of heart disease diagnosis. These findings highlight the technology’s potential for early risk stratification and preventive intervention.
These developments in health monitoring technology parallel other related innovations in the wearable technology sector that are transforming how we approach preventive healthcare.
Predictive Power for Future Health Events
The study’s survival analysis reveals even more compelling evidence of the technology’s utility. After controlling for conventional risk factors including smoking status, BMI, and existing conditions, researchers found that a six-year PpgAge gap was associated with a 46.4% increased risk of atherosclerotic cardiovascular disease events.
Notably, the predictive power of PpgAge gap exceeded that of traditional risk markers. While previous hypertension diagnosis carried a hazard ratio of 1.277 and high cholesterol showed 1.226, the PpgAge gap demonstrated a stronger association at 1.464. This suggests that the technology captures aging-related physiological changes that conventional metrics might miss.
Behavioral Correlations and Lifestyle Factors
The research also uncovered significant associations between PpgAge gap and modifiable lifestyle factors. Smoking status, physical activity levels, and sleep patterns all showed measurable relationships with biological age acceleration. This provides quantitative evidence supporting the connection between daily habits and long-term health outcomes.
These findings complement other industry developments in materials science that are enabling more sophisticated health monitoring capabilities through advanced sensor technologies.
Longitudinal Sensitivity and Clinical Applications
Beyond cross-sectional analysis, PpgAge demonstrated sensitivity to physiological changes over time. The system detected alterations associated with pregnancy and cardiac events, suggesting potential applications for monitoring disease progression and treatment response.
The technology’s ability to track biological aging processes opens new possibilities for personalized medicine and intervention monitoring. As the authors note, “PpgAge is an easy-to-measure aging clock with potential utility in longevity research and translation into clinical practice.”
Implications for Future Healthcare
This research represents a paradigm shift in how we might approach preventive healthcare. The accessibility of PPG data from consumer wearables means that sophisticated health risk assessment could become widely available outside traditional clinical settings.
The study’s findings align with broader market trends toward decentralized healthcare monitoring and personalized risk assessment. As wearable technology continues to evolve, we’re likely to see more integration of such advanced analytics into routine health management.
Furthermore, the technology’s development reflects ongoing recent technology advances in AI and sensor integration that are pushing the boundaries of what’s possible in digital health monitoring.
Limitations and Future Directions
While the results are promising, the researchers acknowledge certain limitations. Prediction accuracy varied across demographic subgroups, and the technology showed weaker associations with some conditions like allergies, asthma, and cancer. Additionally, the study population, while large, may not fully represent global diversity.
Future research will need to validate these findings across broader populations and explore the technology’s utility in clinical decision-making. The researchers also suggest investigating whether interventions that reduce PpgAge gap correspond to improved health outcomes.
As wearable technology continues to advance, the integration of such aging clocks into routine health monitoring could revolutionize how we understand and manage the aging process, potentially extending healthspan and improving quality of life for millions.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.